
Annual report 2018: England, Northern Ireland, Scotland and Wales
Date of publication: October 2018
Our 2018 annual report provides findings relating to people who died by suicide or were convicted of homicide in 2006-2016 across all UK countries. Additional findings are presented on sudden unexplained deaths (SUD) under mental health care in England and Wales.
Our large and internationally unique database is a national case series of suicide, homicide and SUD by mental health patients over 20 years. This allows us to examine the circumstances surrounding these incidents and changes in trends over time, and to make recommendations for clinical practice and policy to improve safety in mental health care.
Key messages
10 key elements for safer care for patients
Our ’10 ways to improve safety’ continue to reflect the evidence we have collected over several years on the features of clinical services that are associated with lower patient suicide rates. These include safer wards, personalised risk management and low staff turnover.

In-patient care
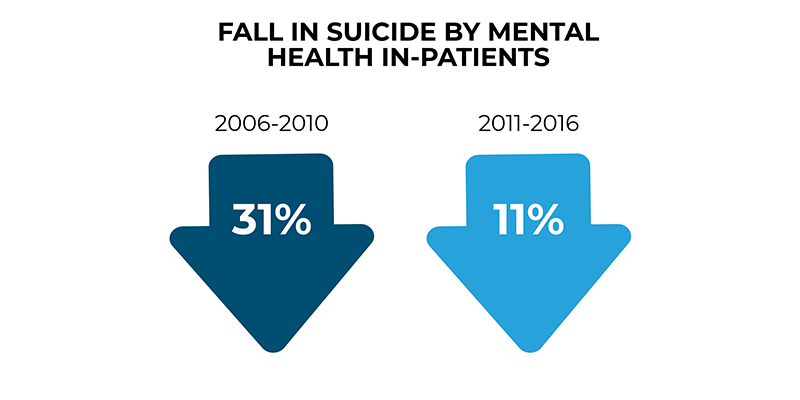
The long-term downward trend in suicide by people under in-patient care has been slower in recent years.
We continue to recommend a renewed emphasis on suicide prevention on in-patient wards, with the aim of re-establishing the previous rate of decrease in in-patient suicide. This could include:
- measures to improve the physical safety of wards, e.g. removing potential ligature points;
- ensuring care plans are in place during agreed leave;
- the development of nursing observation as a skilled intervention.
Service measures to reduce patient suicide risk
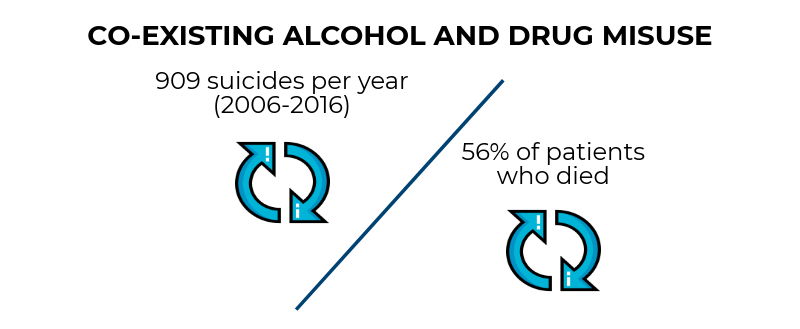
With our findings continuing to show the high risk of suicide in patients (i) recently discharged from in-patient care, (ii) with co-existing drug or alcohol misuse, and (iii) prescribed opiates and opiate-containing analgesics, we emphasis measures that services could take to reduce patient suicide risk:
- follow-up of patients leaving in-patient care within 2-3 days of discharge;
- safe prescribing of opiates and psychotropic drugs;
- reducing alcohol and drug misuse, with specialist substance misuse and mental health services working closely together.
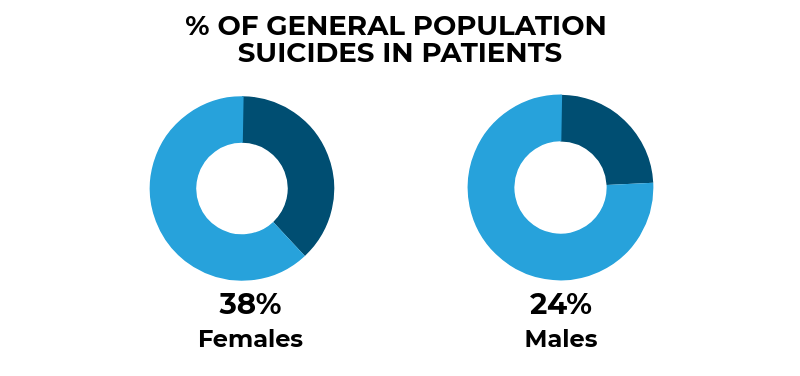
Female patients
During 2006-2016, the number of female patients who died by suicide per year has risen in England but the suicide rate (which takes into account the rising number of female patients under mental health care) has fallen. We have identified a group of female patients who die by suicide who are often younger, with complex problems including self-harm, additional diagnoses and alcohol or drug misuse. We ask clinicians to be aware of the distinct risk profile of female patients who require a particular focus on:
- the treatment of depression, following NICE guidance;
- developing services for self-harm care;
- improving services for people with a diagnosis of personality disorder;
- the care of females with complex problems.
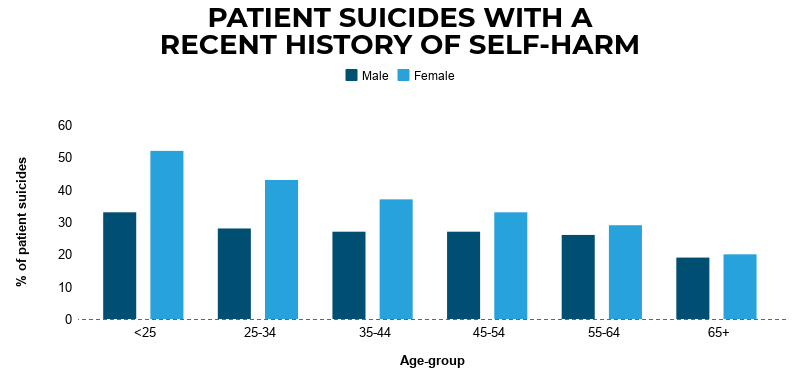
Recent self-harm
Over a quarter (29%) of patients died by suicide within 3 months of self-harm. Self-harm is particularly evident in younger patients. Our findings show an episode of self-harm is common as a recent experience in mental health patients who die by suicide but risk can be under-estimated at assessment. We recommend protocols for managing self-harm patients who are under mental health care highlight the short term risk of future suicidal behaviour.
Young people
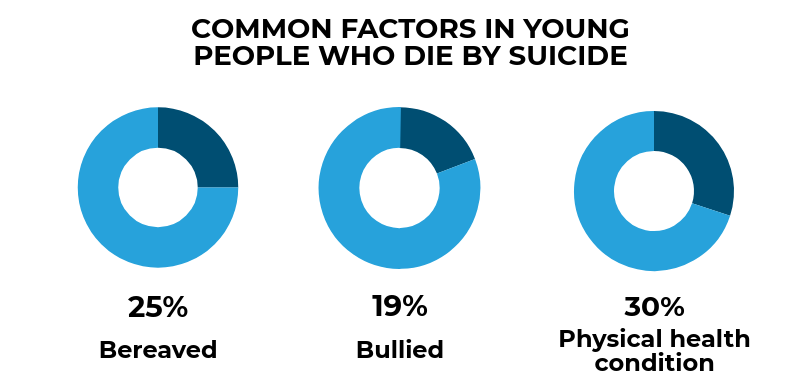
Although the overall suicide rate is falling, suicide in people under 20 is rising. A broad range of stressors appear to play a part, such as family problems, bereavement, bullying, and physical health conditions, reflecting the lives of young people in general. We suggest a wide range of professionals have a role in suicide prevention in young people including those working in self-harm, mental health, social care, primary care, youth justice, education and the voluntary sector.
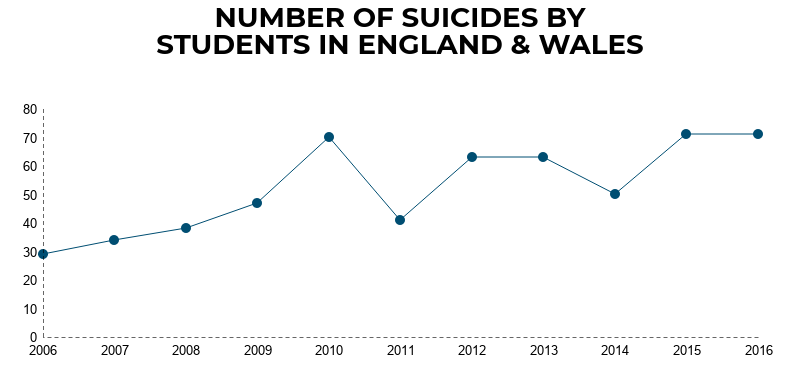
Preventing suicide in students
Our findings show there were 577 suicides in students aged 18-21 in England and Wales, with numbers rising during 2006-2016.
We suggest preventing suicide in students requires specific measures, including:
- prevention, through promotion of mental health on campus;
- awareness of risk, including the fact that conventional risk factors for suicide, such as alcohol or drug misuse, may be absent;
- availability of support especially at times of risk, such as during exam months;
- strengthened links to NHS services, including mental health care.
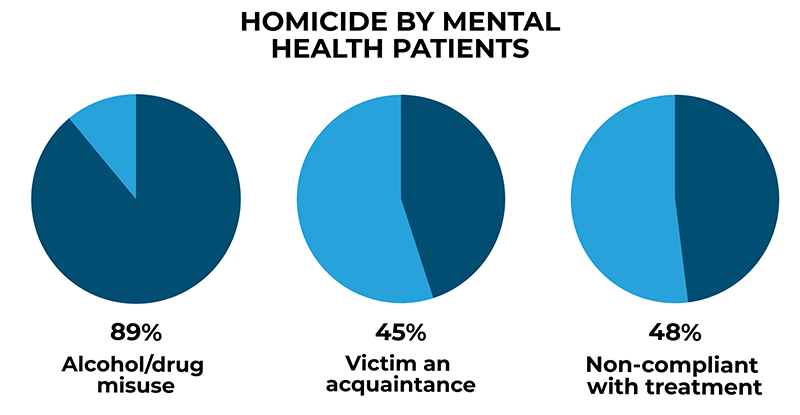
Patient homicide
Since 1997, our findings have highlighted that the risk of homicide by mental health patients is related to the use of alcohol or drugs rather than from mental illness itself, and to people who are known to the patient – stranger homicides are rare. We have shown around half of patients were not receiving care as intended and patients were also at high risk of being victims of homicide.
We recommend the clinical measures most likely to help services prevent interpersonal violence are:
- reducing alcohol and drug misuse;
- maintaining treatment and contact in patients at risk of losing contact with services.
Icons made by Freepik from www.flaticon.com is licensed by CC 3.0 BY
