Cancer
The University of Manchester’s approach to cancer research spans the full spectrum of combating the disease.
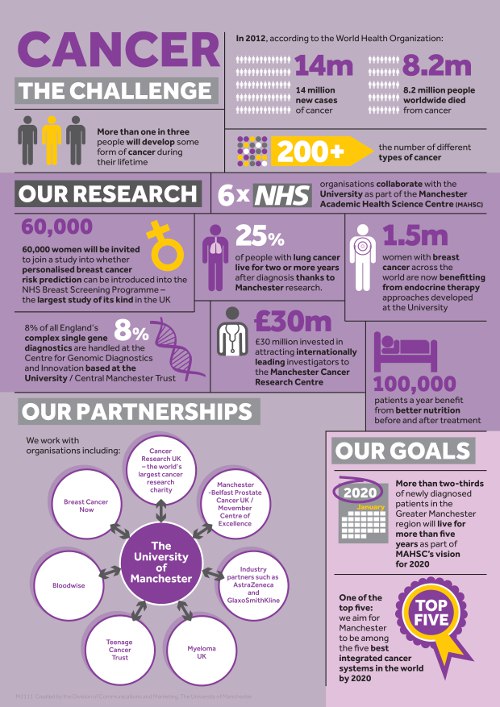
One in two of us will be diagnosed with some form of cancer during our lifetime. Cancer may be one illness, but there are over 200 types – and a diagnosis affects whole families.
Breadth of our research
One in Two: a Manchester cancer research podcast
Stream the latest episodes of our podcast made in partnership with the Manchester Cancer Research Centre (MCRC).
The University of Manchester’s medical research ranges from understanding the molecular and cellular basis of cancer to the development and testing of novel drugs and other therapeutic approaches.
Through nursing, psychology and policy work, solutions to the physical, emotional and economic impacts of cancer are being researched and put into practice across the University.
Led by world-renowned scientists such as Professors Robert Bristow, Caroline Dive and Gareth Evans, cancer research at the University has the academic strength to match the weight of our partnerships and the benefits of our location.
The expertise and facilities available in Manchester can prove vital in the fight against cancer. We have a responsibility to share our knowledge, and our work in Africa is just a small distillation of our impact globally.
Rob Bristow / Professor of Cancer Studies
Making a difference
As the UK’s first university to set social responsibility as a core goal, we’re committed to delivering research that transforms people’s lives and creates positive change across the world.
We’re contributing to improving the evidence base for the treatment and detection of cancer in the UK and forging global partnerships in Africa and other countries as part of our ‘precision cancer medicine for all’ approach.
We know the value of working together with others. We break down barriers and get involved; we collaborate across disciplines, cultures and countries to solve global problems.
Reach and impact
Our links with NHS organisations and cancer charities – as well as the support of the local population – make for an unrivalled beacon of research, where outstanding clinical work is leading to innovative techniques and personalised treatments.
Through the Manchester Cancer Research Centre we work with Cancer Research UK and The Christie NHS Foundation Trust to turn research findings in the laboratory into better, more effective, treatments for cancer patients. The Centre’s new building houses 150 researchers and world-class facilities for imaging and sample analysis.
Our trials led to anastrozole replacing tamoxifen as the major endocrine therapy for breast cancer, a development that has benefited 1.5 million women globally. Our partnerships with companies such as AstraZeneca and GlaxoSmithKline bring new drugs to the market.
And we’re reaching out to where help is needed most – such as in Uganda, where our academics and medics are helping to roll out a national programme of cervical cancer screening.
Cancer is a disease that affects so many, in different, often devastating, ways. At The University of Manchester we want to loosen cancer’s grip and improve the lives of those it affects.
Global challenges, Manchester solutions
Saving children’s lives across the globe
Global challenge
Leukaemia is the most common cancer in children and teenagers, and acute lymphoblastic leukaemia (ALL) is the most common type of childhood leukaemia. ALL is a particularly rapid and aggressive form of cancer requiring immediate treatment.
Manchester solution
Our researchers have made a significant contribution in the UK, which now has an 85% cure rate for childhood ALL, one of the highest in the world. Direct results of our research in ALL also include a 10% improvement in outcomes for relapsed cases in the UK, the Netherlands, Australia and New Zealand. Changes in clinical practice based on our research are now national standards of care for children with ALL in the UK and Ireland and our relapse protocol underpins European practice. Our researchers have increased survival rate of the disease by 15% in India in just five years.
Fighting the obesity epidemic
Global challenge
Being overweight or obese is the second biggest preventable cause of cancer in the UK after smoking, contributing to around 18,100 cases of cancer every year. More than 60% of the UK population is categorised as obese and this is expected to increase.
Manchester solution
Manchester researchers were the first to prove a link between weight gain and cancer, identifying that obesity is directly linked to 20 different types of the disease. Recently, we have shown that increased weight in childhood is linked with increased risk of bowel cancer later in life. This knowledge is now being used by public health professionals and clinicians globally to increase awareness of the role of a healthy diet and lifestyle in preventing cancer.
Improving radiotherapy
Global challenge
Radiotherapy plays a major role in cancer therapy. However, the individual nature of a patient’s cancer makes it difficult to accurately target the therapy. Tumour tissue can be missed and unnecessary side-effects caused.
Manchester solution
Manchester is home to the UK’s first high-energy NHS proton-beam therapy centre, where researchers and clinicians work in parallel to better tailor and target radiotherapy. We’re improving understanding of the errors and variation in treatment planning, and using real-time imaging to help adapt personalised therapy plans as tumours shrink or move. This will improve outcomes for patients in terms of survival and quality of life.
Preventing breast cancer
Global challenge
Breast cancer is the most common cause of cancer and cancer mortality in women worldwide. Nearly 1.7 million new cases were diagnosed in 2012, representing 25% of all cancers in women.
Manchester solution
We have developed new approaches to endocrine therapy – treatment that blocks the body’s natural hormones – for breast cancer in postmenopausal women. Our work has increased the duration of survival of women with advanced breast cancer, reduced relapse rates and improved survival after surgery for early breast cancer. It has also successfully prevented disease in women considered at high risk.
Saving lives through earlier detection
Global challenge
Mortality rates for lung cancer are the highest of all cancers as diagnosis generally happens at an advanced stage. Early detection of the disease is necessary to increase survival rates.
Manchester solution
Our innovative mobile screening project, which located mobile screening units in supermarket car parks in traditionally hard to reach areas, found one case of cancer for every 33 detected, a threefold increase compared to conventional approaches. Our novel approach, targeting the traditionally hard-to-reach populations, improving lung cancer survivorship by detecting lung cancer earlier and has demonstrated an ability to shift diagnosis from late to
early stage disease, resulting in more lives being saved.
Developing new treatments
Global challenge
Clinical trials are essential for introducing new treatments and developing better standards of care across all types of cancer.
Manchester solution
We are home to the world’s largest early-phase clinical trial treatment unit and are world leaders in conducting clinical trials. Our pioneering study of gemcitabine and platinum helped establish the regimen as the standard first-line treatment of advanced non-small cell lung cancer (NSCLC) in Europe, and at the turn of the century we treated the first-ever NSCLC patient with gefitinib, paving the way for a new era of personalised treatments for lung cancer.
Liquid biopsies for lung cancer
Global challenge
Lung cancer has one of the lowest rates of cancer survival: fewer than 10% of patients survive five years after diagnosis. More targeted therapies are needed but the biopsies required to profile patients’ tumours are invasive and not without risk.
Manchester solution
Manchester has world-class expertise in blood-borne biomarkers. By detecting and characterising tumour cells circulating in the blood, we can identify faults, target them with smart drugs and then select the most appropriate treatment all without the need for surgery. We can create patient-relevant laboratory models to test new therapeutic strategies and to better understand mechanisms of resistance and relapse.
In-depth insight
Get an in-depth insight into some of our world-changing cancer research.
Read more
On Cancer
Our publication On Cancer provides expert analysis and thought leadership on cancer prevention, diagnosis, and treatment.
Read the full publication
Cancer research at Manchester
Find out more about cancer research at the Faculty of Biology, Medicine and Health.
Visit the Faculty of Biology, Medicine and Health website
Research beacons breakthrough ebook
Read our ebook for insights into how Manchester commercialises its world-class academic research.
Download our breakthrough ebook
Manchester Cancer Research Centre
The MCRC was formed in 2006 by the University, CRUK and The Christie NHS Foundation Trust.
Visit the MCRC website
Cancer Research UK Manchester Institute
A leading cancer research institute within the University, core funded by Cancer Research UK.
Visit the CRUK Manchester Institute website
Events
-

A Community Event on Teamwork in Research
14 May 2024, 12pm-2.30pm
Hosted by The Team Research Programme, funded by Research England, who aim to increase awareness of the Team Research (Team Science) interdisciplinary model and its value to resear.. -

MBC Seminar: Gerald Lip "AI in breast cancer screening - are we there yet?”
24 May 2024, 3pm-4pm
Manchester Breast Centre (MBC) External Seminar Series, sponsored by Breast Cancer Now Friday 24th May, 2024, 3:00pm – 4:00pm Dr Gerald Lip, Clinical Director North East of Sc..

.jpg)