.jpg)
Dr Hannah Harrison uses a novel cell culture system to reveal how breast cancer creates perfect conditions for it to spread in the body – and how we can stop this from happening.
Breast cancer is the most common cancer in women in the UK, with 1,000 people a month dying from the disease. This is mostly from cancer spreading to other parts of the body – a process known as metastasis. Secondary tumours from metastasis in places such as the lungs, liver, brain, and bones also cause symptoms that can significantly affect people’s daily lives.
Scientists attempting to understand metastasis have learnt that these secondary sites are not passive in this process but, in fact, sometimes help metastatic breast cancer cells to survive and multiply. Breast tumours release chemical signals into the blood that alter the environment before cancer cells reach the secondary site and make the area more favourable for them to live. It’s as if cancer cells are picky guests at a hotel, sending advance notice of what they’ll need in their room when they eventually arrive.
Dr Hannah Harrison, a University of Manchester Post-Doctoral Fellow based at the Manchester Cancer Research Centre, has been studying this communication between breast tumours and secondary sites in the body. “Secondary breast cancer is a massively under-studied and under-funded part of the disease,” Dr Harrison says, “it's something that people don't like to talk about because it's incurable.”
A new option for growing cells in a lab
It's about finding a way to make it a chronic disease, meaning that patients can live a long life without pain and other symptoms of metastatic disease.
Dr Hannah Harrison / Division of Cancer Sciences
Dr Harrison’s latest work involves using a cell-culture system called Quasi-Vivo®. In this system, cell culture liquid is pumped between interconnected chambers that help different cell types in the chambers grow and carry messages between them (as well as cancer cells that can break away). While it’s relatively simple to set up and run, the process can be customised in complex ways to answer questions that other lab-based methods can’t.
The first Quasi-Vivo® system Dr Harrison encountered belonged to an old supervisor of hers, who had bought it to try and grow bone samples in the lab. However, she felt “it never achieved its full potential.”
Later, Dr Harrison came across a researcher in Sheffield who was using the Quasi-Vivo® system to grow cells called fibroblasts, which can sometimes support tumour growth. She also looked at the work of Professor Arti Ahluwalia from the University of Pisa in Italy, who had developed and validated a method for in vitro culture of simplified tissue models where multiple cell types (representing different tissues and organs) are cultured to appropriately scaled ratios to represent the tissue of interest. Professor Ahluwalia found that the Quasi-Vivo® system more closely resembled the results of tests in mice than other lab-based methods.
Dr Harrison applied for and won funding from the NC3Rs and Cancer Research UK to adapt Prof Ahluwalia’s system for her own research into breast cancer metastasis.
Understanding the difference between breast cancer and other parts of the body
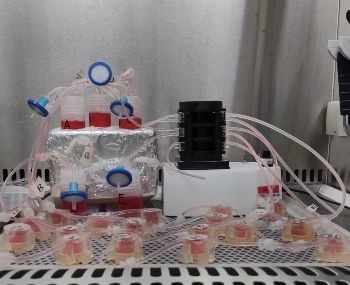
After spending some time optimising how to grow breast cancer cells in the Quasi-Vivo® system, Dr Harrison has looked at how these cells are attracted to secondary sites such as the lung. Blocking the activity of certain proteins (either by knocking out the genes which produce them or with drugs) will allow her to unpick the complex conversation happening between breast cancer cells and lung cells. In turn, she plans to expand these experiments to look at other major sites for breast cancer metastasis, including the liver, bone, and brain.
In future experiments, she plans to delve further into exactly what chemical signals the cancer cells are sending out to the rest of the body. This knowledge could eventually help researchers find ways to interfere with the communication between cancer cells and secondary sites and stop metastatic cancer cells from growing into tumours at all.
Reducing the use of mice
The Quasi-Vivo® system has replaced a lot of experiments Dr Harrison might otherwise do with mice, and she believes other breast cancer researchers could do the same. To help demonstrate its value and get it adopted more widely, she is planning collaborations with leading researchers from across Europe and the US, aiming to replicate the findings of their mouse experiments using the Quasi-Vivo® system. In all, Dr Harrison estimates her model system could reduce the number of mice used in experiments by thousands each year.
Improving breast cancer research
Dr Harrison believes the Quasi-Vivo® system will allow scientists to answer some of the burning questions about breast cancer metastasis in much more detail and on a much larger scale than other methods. “With the Quasi-Vivo®, I think we’ll be able to develop a model where you can ask those questions, and that in itself will drive the discovery forward more quickly to achieve a better outcome for patients”, Dr Harrison says.
It's this potential for people suffering from breast cancer which motivates her most; through understanding breast cancer metastasis with the help of her Quasi-Vivo® system, her hope is that we can turn metastatic breast cancer from something that kills 1,000 women every month, into something that can be controlled and contained. “It's about finding a way to make it a chronic disease, meaning that patients can live a long life without pain and other symptoms of metastatic disease .”
