
Applying Manchester’s pandemic expertise in Kenya
A team from The University of Manchester has been sharing their clinical experience from working on the frontline during the coronavirus outbreak with colleagues in sub-Saharan Africa to help implement significant public health changes.
The multidisciplinary initiative involves experts from the University’s Faculty of Biology, Medicine and Health, the Faculty of Humanities and the Faculty of Science and Engineering.
Building on the extensive collective experience in areas related to poverty, urban health, informal settlements and inequality in the Global South at the Global Development Institute and the Division of Population Health of the University, the group developed a partnership with key institutions in Kenya.
These included the Adventist Development and Relief Agency, African Population Health Research Centre, Kenya Medical Research Institute, Slum Dwellers International and several Kenyan universities. The purpose of the partnership is to develop and deliver a research agenda focused on COVID-19 prevention in the informal settlements in Kenya.
A University-wide approach
University colleagues successfully bid for funding from the Global Challenges Research QR Funds to initiate a formal study around the effectiveness of wearing face masks in large informal settlements – referred to locally as slums.
The pilot study is currently being conducted at three large informal settlements in Nairobi, Kissi County and Nakuru County. Members of the Kenyan diaspora in Manchester, led by Mr John Gutto, have helped the University team to build partnerships and links with these settlements in a relatively short time period.
The study, which concludes in December 2020, has been managed on the ground by University field teams who have engaged with 200,000 shanty dwellers to date. The field teams have been communicating simple World Health Organization-approved public health messages and have distributed 45,000 reusable face masks for free.
Despite these financially challenging times, The University of Manchester committed £100,000 to support this project in Kenya, which is a reflection of the institution’s social responsibility priority.
In this first phase, the team looked at the knowledge, skills and attitudes that currently prevail within these informal settlements on aspects related to the use of face masks, not how their use is affecting transmission, as that will be explored in phase two of the study.
Following the pilot, the University intends to apply to the National Institute for Health Research to evaluate the effectiveness of a multi-model public health care bundle to prevent or reduce the transmission of acute viral diseases with pandemic potential. This study is likely to extend across multiple countries in East Africa, especially Kenya and Uganda.
Positive effects of multidisciplinary working
The experience of working with patients with severe forms of COVID-19 at Manchester Royal Infirmary provided members from across the University’s three Faculties with a serendipitous opportunity to share some of their own experiences with colleagues in Kenya and in Uganda.
Despite some enormous challenges at home, the team, led by Professor Mahesh Nirmalan, have used the well-established contacts and links between Manchester, Kenya and Uganda to initiate some important discussions on the management and prevention of coronavirus diseases that have led to substantial changes in these countries.
These discussions resulted in the research project funded by the University aimed at developing strategies to prevent the spread of COVID-19 infections in crowded informal settlements in sub-Saharan Africa.
From cancer care to coronavirus
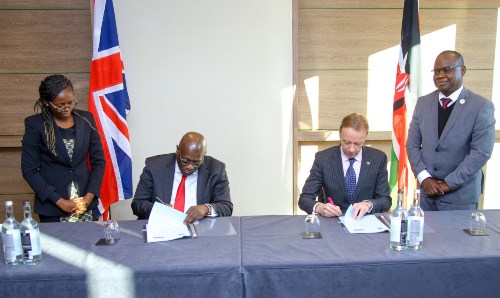
In January 2020, the University and The Christie NHS Foundation Trust signed a Memorandum of Understanding to collaborate with Kenyatta University Teaching, Research and Referral Hospital in the prevention and management of non-communicable diseases, with a special emphasis on cancer and mental health.
The agreement provides training and exchange opportunities of health professionals, including Kenyan nurses, who will get an opportunity to work in Manchester.
As the coronavirus epidemic started, questions were being asked whether the virus would have the same ferocity in Africa. The partnership has allowed the University to provide colleagues in Kenya with insight around what was happening in Manchester and some of the challenges faced here, including working with limited resources such as personal protective equipment.
This led to implementing some essential primary care interventions in Kenya to prevent the spread of the virus within African populations. In some informal sub-Saharan African countries, there is extreme crowding. It was recognised by the World Health Organization and other authorities that if the virus took hold within these settlements it would result in a major human catastrophe.
“The University and clinicians in Kenya have been trying to find solutions to manage the coronavirus and have been discussing the possible preventative and isolation measures needed,” says Professor Nirmalan.
“As a group, we’ve spoken about the level of preparedness the Kenyan government is initiating in terms of providing oxygen treatment to large numbers of people.
“I felt quite privileged to have been involved in those discussions and as a result, we have catalysed a shift in thinking with a focus on prevention and primary care. Our discussions also focussed on developing capacity to provide simple oxygen therapy simultaneously to several unwell patients rather than the undue emphasis given by the Western media to the acquisition of new ventilators and ventilation strategies in these settings.
“Implementing the wearing of face masks or informal face coverings and increased spacing between subjects isolated in isolation centres have also been the focus of these discussions and have now been incorporated into the strategy adopted by the Kenyan government.”
Knowledge sharing with international peers
After caring for acutely ill patients in Manchester, the University was in a position to share experiences with colleagues in Kenya to help them manage the current pandemic through treatment and prevention.
Colleagues across the University used this opportunity to undertake the ambitious, in-depth study on the prevention and reduction of viral transmissions within crowded settlements. As an example, the role of Faculty of Science and Engineering was to look at novel materials for the construction and design of face masks.
In another example, the Global Development Institute is looking at regional value chains (the most cost-effective way) in East Africa to source the best materials to make face masks, find reputable manufacturers and engage with the best distributors at a time of a future pandemic.
“This truly is a multidisciplinary project trying to look at the effectiveness of this public health care bundle we have put together, whether it can be used now or in future pandemics in crowded settlements in Africa, South America or South East Asia,” says Professor Nirmalan.
“Preliminary work is currently underway and we’re excited to continue working with the University of Nairobi, Kenya Medical Research Institute, Egerton University and the Kenyan diaspora in Manchester who have enabled us to establish invaluable links with Kenya.
“Following the pilot's success, we hope it will form the basis of a much bigger project across the whole of Kenya, Uganda and other East African countries and look at the impact of a multifactorial public healthcare bundle to prevent or slow down the transmission rates of acute viral diseases of pandemic potential in the future.
“Greater Manchester has a history of vaccine trials and neurological studies. This particular multidisciplinary research team has brought global health as an important dimension in the overall COVID-19 response to the University and across the region.”
How legacy outreach clinics in Uganda are supporting work in Kenya
Dr Jonathan Huck and Professor Nirmalan have been working closely since 2015.
Their research in Gulu, northern Uganda, was supported by Medical Research Council grants and following the Ugandan civil war, they helped to establish the first outreach artificial limb clinics in the region. In 2019, the professors delivered more than 50 artificial limbs to people who had never received them before.
Professor Huck initiated a programme to map some of the most remote and unmapped areas in that part of the world. That experience has enabled the team to utilise those networks in the study taking place currently in Kenya, which in turn is helping to raise the University’s profile in sub-Saharan Africa.
Tackling the world’s most recent pandemic has required new ways of thinking. The truly international, interdisciplinary approach of the team at Manchester is helping to ensure that the lessons learnt are shared for the good of communities around the world.
Meet the researchers
- Professor Mahesh Nirmalan, Vice Dean for Social Responsibility and Public Engagement
- Professor Diana Mitlin, Professor of Global Urbanisation
- Professor Keith Brennan, Professor of Developmental Signalling
- Dr Jonathan Huck, Lecturer in Geographical Information Science
- Professor Arpana Verma, Clinical Professor of Public health and Epidemiology
- Dr Tucker Gilman, Senior Lecturer in Earth and Environmental Sciences

